12332 Bear Plaza Suite 100 Burleson, TX 76028
reception2@ipsdfw.net
(817) 615-8840
Fda Approves Scs Device For Painful Diabetic Neuropathy

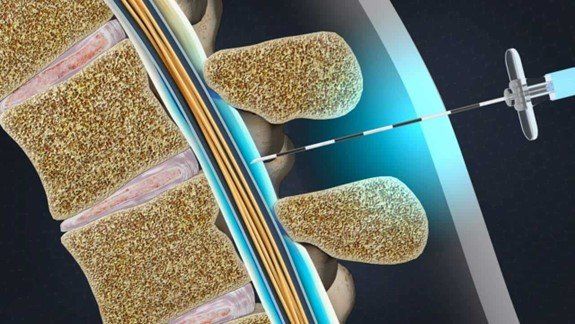
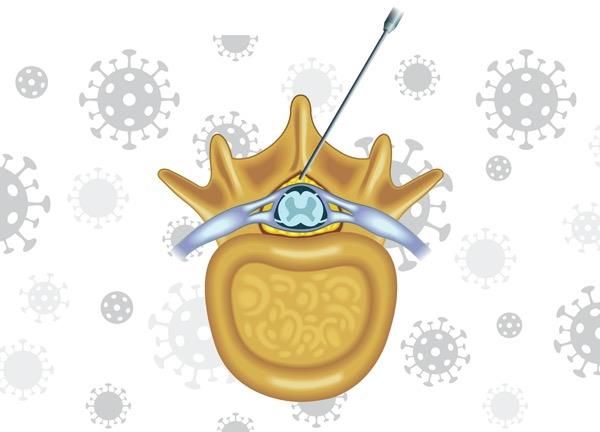
The FDA
expanded its approval for a spinal cord stimulation (SCS) device to include an indication for painful diabetic neuropathy (PDN). The approval follows the high-frequency device’s (Senza, Nevro) positive clinical trial results, recently published in JAMA Neurology (2021;78[6]:687-698).
The trial found that at three months, 79% of participants (N=216) receiving SCS treatment alongside conventional medical management reported at least 50% improvement in visual analog scale (VAS) scores without worsening neurologic deficits, compared with 5% of participants receiving conventional management without SCS (P<0.001).
At six months, the mean VAS score for the SCS group dropped from 7.6 (95% CI, 7.3-7.9) to 1.7 (95% CI, 1.3-2.1), while the scores stayed the same for those treated without SCS, beginning at 7 (95% CI, 6.7-7.3) and finishing at 6.9 (95% CI, 6.5-7.3).
Along with the changes in pain scores, the researchers also noted neurologic exam improvements in 62% of the SCS participants at six months, compared with 3% of the patients receiving conventional management alone (P<0.001).
Primary investigator Erika Petersen, MD, FAANS, FACS, a professor of neurosurgery at the University of Arkansas for Medical Sciences College of Medicine, in Little Rock, reported that her team also witnessed improvements in ambulation, specifically in walking tests, where patients in the SCS arm made gains and walked further after treatment periods, while the conventional management arm did not.
“It’s one thing to say [a patient’s] pain level is lower, but if somebody [a patient] can actually do more because of the pain being better controlled than that, it really translates to improved overall function,” Petersen said in a previous conversation with Pain Medicine News.
“In Arkansas, where we have many patients with diabetes and PDN, we were determined to study a non-pharmacological treatment like SCS where few other options are effective,” she said in an email.
“These findings were tremendous steps forward for the field of neuromodulation,” Petersen said late last year. “The fact that 10-kHz SCS does not generate paresthesias is beneficial when considering SCS for diabetic neuropathy, as many of these patients experience tingling sensations at baseline and do not tolerate added paresthesias.”
Our Recent Articles


Get In Touch
Please fill out the service inquiry form and we’ll get back to you. If you require immediate assistance, please contact us via telephone or email.
We will get back to you as soon as possible.
Please try again later.
Through comprehensive exams and medical history, Dr. Vyas will focus on developing a treatment plan that is right for you.
Useful Links
CONTACT INFO
12332 Bear Plaza Suite 100 Burleson, TX 76028
(817) 615-8840
reception2@ipsdfw.net
All Rights Reserved | Interventional Pain & Spine
Website Design by Viral Growth Marketing + Design

