Are you experiencing ongoing neck and/or back pain? Have oral medications, physical therapy, or other treatments failed to help? You may benefit from minimally invasive epidural injections.
Clinical research studies have indicated that Epidural Steroid Injections (ESI) relieved back pain more effectively than other conservative therapy.
Would you like to find out more about these treatments? The following guide will explain this procedure and some of it’s benefits.
How Do Epidural Steroid Injections Work?
Steroids are powerful anti-inflammatory medications. This means that they work to decrease swelling.
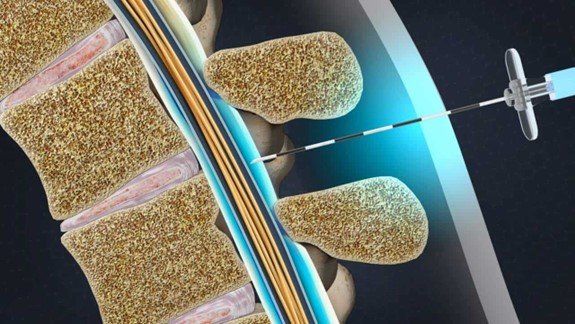
The epidural space describes the area outside the sac of fluid around the spinal cord. Providers inject steroids and anesthetics into this area.
The goal is to decrease swelling that’s pushing on the spinal cord and nerves. Compression in these areas creates pain, numbness, tingling, and weakness.
Reasons To Get An Epidural Injection?
Epidural Steroid Injections are used to safely treat many back, neck, and nerve pain conditions. This allows individuals to resume their normal activities. For some, this may be part of a combination of treatment, including physical therapy.
Some of the various reasons that providers choose ESI include:
- Avoiding or delaying the need for surgery
- Decreasing the amount of pain medication you’re taking
- Decreasing the number of inflammatory markers that increase pain
- Increasing your mobility and daily function
- Relieving neck pain that spreads to your arms
- Relieving back pain that spreads down your hips and legs
Pressure on your spinal cord and nerves can result from several conditions. These include bulging disks, slipped vertebrae, bone spurs, thick ligaments, and joint cysts. Arthritis in the spine can lead to a thickening of the spinal ligaments and compression.
Epidural Injection Tips For Before The Procedure
Make a list of questions to ask your provider so you don’t forget to ask anything in their office. Here are some ideas to get you started:
- The name of the procedure?
- How this procedure can help your condition?
- Benefits and the risks?
- Possible complications or side effects?
- Who will perform the injection?
- Where will the procedure take place?
- Will you go home the same day?
- How long will it take to see results?
- What to do if you have questions or concerns when you get home?
During your visit, be sure to tell your provider if you’re pregnant or plan to become pregnant. Also, describe all your medical conditions such as diabetes or an allergy to contrast dye. Bring a complete list of all medications, supplements, or antibiotics you’re taking.
Be sure to tell them if you take medicines that thin your blood. Examples include aspirin, naproxen, heparin, ibuprofen, warfarin, and clopidogrel.
These could increase the risk of bleeding after the procedure. Your provider may have you stop taking these medicines for a few days before the injection.
The Experience of Epidural Injections Explained
Epidural injections often take place in doctors’ offices, surgical centers, or hospitals. Most patients go home on the same day.
Providers with specialized training administer these injections. Examples include anesthesiologists, neurologists, physiatrists, and spine surgeons. Pain and spine management experts also provide this treatment.
Before the procedure, your provider may give you medication to help you relax.
Your injection site determines how you’ll be positioned for the injection. Most commonly, patients lie face down with a pillow underneath your stomach. You may also lie on your side in a curled position or sit up.
The area is cleaned with special soap, called Betadine or Chloraprep, which feels cold on your skin. This decreases the risk of infections. They’ll often inject numbing agents into and just below the skin to reduce discomfort. This may sting at first before it makes the area numb.
Next, the doctor will insert the needle. Most commonly, they use real-time video X-rays to see exactly where the needle is going. Once the needle is in the epidural space, they’ll inject steroids and numbing medicine.
You may feel pressure, tingling, or burning during the medication injection. Most patients don’t feel pain. It’s important to stay still so that the needle stays in the right place.
After the injection, the provider removes the needle and applies a dressing.
Post-Procedure Expectations
The staff will watch your vital signs for 15 minutes to an hour after the procedure. Once you’re feeling awake, you’ll be sent home. You’ll need to avoid driving and air travel for the remainder of the day.
It’s not uncommon to feel some discomfort at the injection site for a few hours. Ice packs work well to improve your comfort. Your provider may ask you to rest and avoid strenuous activity for the rest of the day.
Some patients experience increased pain for two to three days after the procedure. This isn’t uncommon since it takes about that long for the steroid to take effect. Most people feel pain relief 48 hours to a week later.
Epidural injections can reduce pain for weeks, months, or a year. Unfortunately, some patients may not achieve pain relief and need to explore other treatments.
Possible Epidural Injection Side Effects
Side effects following epidural injects aren’t usually serious. Examples include dizziness, headache, and nausea. The steroid can cause the following symptoms:
- Anxiety
- Face and chest flushing
- Increased temperature
- Menstrual changes
- Trouble sleeping
- Water retention
Some people experience anxiety with the procedure, which can lead to fainting. These symptoms usually get better with rest.
If you develop more serious problems, it’s important to call your doctor at once. For example, look out for increased redness, swelling, heat, and pain at the injection site. Also, call for increased numbness or weakness in your arms or legs, or if having trouble breathing.
These signs may indicate a serious or rare complication such as medication reactions, infection, bleeding, or brain and nervous system issues.